



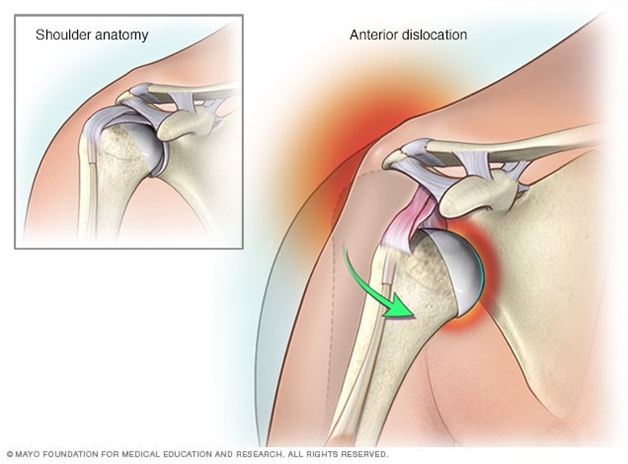

Shoulder dislocation means the head of the humerus (the ball) is completely displaced out of the glenoid (the socket). Shoulder subluxation means a ‘partial dislocation’ where the ball only slips out partially out of the joint and slips back into position again.
Shoulder is one of the most mobile and the least stable of all the joints in the body. This makes it the joint which is most vulnerable for dislocations or subluxations. In a proportion of these patients, the shoulder tends to dislocate or subluxate repeatedly after the first dislocation. Patients with a tendency for recurrent (repeated) dislocation or subluxation are said to have an unstable shoulder or shoulder instability.
A shoulder may dislocate after a significant injury like a fall on an outstretched hand or due to a direct blow to the shoulder (traumatic dislocation), or it may dislocate without a significant injury (atraumatic dislocation) in patients who have an inherent laxity of joints (loose jointed patients). In some patients like throwing athletes, the repetitive action of forceful throwing causes the anterior capsule to stretch out and can eventually lead to a dislocation or subluxation (microtraumatic dislocation).
Shoulder dislocation is classified on the basis of the direction in which the ball dislocates in relation to the socket. It is termed unidirectional if it dislocates in one direction only, or multidirectional if it dislocates in more than one direction. Thus there are the following types of dislocation:
a. Anterior – the ball dislocates in front of the socket. This is the commonest type.
b. Posterior – the ball dislocates behind the socket
c. Inferior – the ball dislocates below the socket
These are usually atruamatic in nature and occur in patients who have inborn laxity in their joints.
Recurrent dislocation implies having repeated dislocations of the shoulder. Patients with a tendency for recurrent (repeated) dislocation or subluxation are said to have an unstable shoulder or shoulder instability (unstable shoulder). Shoulder instability may follow after a traumatic dislocation (after a fall or injury to the shoulder), due a generalized laxity of ligaments, or due to gradual stretching of the joint capsule due to a repetitive injury as in a throwing athlete.
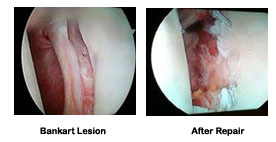
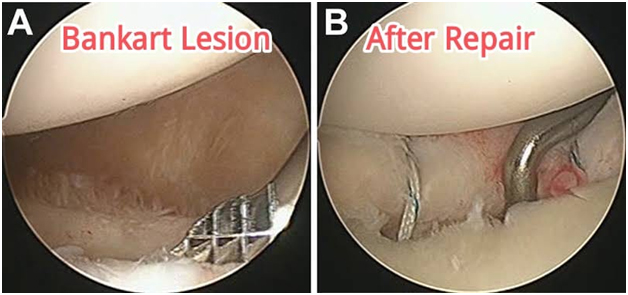
When the shoulder dislocates in the front (anterior dislocation) because of an injury, the ball (head) is forced out of the joint (socket). This causes disruption of the labrum, capsule and the ligaments in the front of the shoulder. This is known as the Bankart’s lesion. The head of the humerus (ball) comes to lie over the front edge of the glenoid (socket) and this causes an indentation on the ball. This is known as the Hill-Sach’s lesion.:
In a proportion of patients the Bankart’s lesion does not heal completely causing the joint to be unstable and vulnerable to further dislocation with trivial trauma or no injury. It is now a well known fact that the younger the patient at the time of first dislocation (age less than 25 years), has higher chances of re-dislocation. The chance of shoulder re-dislocating after the first dislocation can be as high as 70-90% in a young patient (below 25 yrs of age). With each dislocation the capsule in the front gets stretched and thinned out making further dislocations to happen occur with relative ease. On the other hand, in patients with an inherent laxity of the joint capsule, the joint is capacious (lax) and is easily dislocated with trivial injury or during activities like throwing or wearing a shirt.
Shoulder instability is diagnosed on the basis of patient’s symptoms and physical examination. Shoulder instability could present with history of repeated episodes frank dislocations causing pain or discomfort. Most of these patients are able to reduce (put back the dislocated shoulder) on their own or with some assistance. Some patients may present with pain or discomfort while moving the shoulder without an obvious dislocation. This is due to the shoulder being subluxed (partially dislocated) instead of a complete dislocation. This usually occurs in the throwing position (abduction and external rotation of the arm) in athletes or while doing activities of daily living like putting on a shirt or lifting a heavy object. Physical examination will reveal an otherwise normal shoulder. The only positive finding is the ‘apprehension test’. In this test the arm is put in the vulnerable position of abduction and external position. This will cause pain or discomfort and the patient becomes apprehensive that the shoulder will re-dislocate. In patients with ligament laxity, episodes of dislocation or subluxation will occur without any significant injury. Further, since they have generalized ligament laxity, they may present with symptoms in both shoulders (bilateral dislocations or subluxations). Also these patients may exhibit evidence of laxity (loose-jointed) in the form of repeated patellar (knee cap) dislocations or hyper-extended knees. These patients will also have a positive ‘apprehension test’ on examination.
There are certain tests which may be performed to gain further information and plan out the treatment.
These are helpful only in patients with a frank dislocation where it demonstrates the presence of a dislocated head. In cases with recurrent dislocation certain special views will demonstrate the Hill-Sach’s lesion (indentation at the back of the head). Otherwise X-rays are not of much value.
This will clearly demonstrate the Bankart lesion (which is diagnostic of a recurrent dislocation) as well as the Hill-Sach lesion. In patients with ligament laxity, arthrography reveals a very capacious joint with a lax capsule.
This is very useful in demonstrating any bone loss in the glenoid socket. The amount of bone loss in the glenoid will dictate the type of surgical procedure to be performed.
When a shoulder dislocates it must be promptly relocated by closed reduction (manipulating the shoulder without the need for open surgery). This may require a general anaesthetic or some form of sedation. Once the shoulder is relocated, the arm is immobilized by the side of the chest using a shoulder immobilizer type of sling for a period of 3-6 weeks. In very young patients (below the age of 25 years) and high demand athletes, there may be a case need for surgery (Bankart repair) immediately after the first dislocation to prevent the chance of further dislocations as the incidence of recurrent dislocation in these patients is very high.
The treatment options for repeated shoulder dislocations depend on the functional demands of the patient and the level of disability suffered by the patient due to these episodes of instability.
Those patients who have a sedentary life-style and those who are not involved in strenuous activities or active sports may be able to manage without surgery as long as they are able to restrict activities which are likely to cause a dislocation or subluxation. However, there is an ever present risk of dislocation or symptomatic instability occurring at any point in time if the shoulder is placed in a vulnerable position.
Most young patients and those involved with any type of active sport are likely to need surgery to stabilize their unstable shoulder. The commonly used surgical options are:
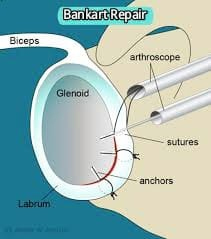
Arthroscopic Bankart repair (Key-hole surgery)
This is performed through 3 small holes (called portals). The Bankart repair involves re-attaching the detached capsulo-labral complex to the glenoid using suture anchors. It is also possible to do a capsular shift (tightening of the lax capsule) at the same time. The advantage of the arthroscopic technique is its minimally invasive nature which minimizes morbidity of surgery and hospital stay. Further it allows excellent visualization of the entire shoulder joint and is very useful in detecting and treating other causes of dislocation like a SLAP lesion.
Open Bankart Repair
The Bankart repair and capsular shift can also be performed by open surgery which involves making a cut of about 3-5 cm over the front of the shoulder. This procedure also involves cutting through the subscapularis muscle which needs to be repaired at the end of the procedure.
Bony operations
In cases where there is significant bone loss in the glenoid or a large Hill-Sach’s lesion (engaging Hill-Sach’s), a Bankart repair alone is likely to fail. In such situations a Bristow-Latarjet procedure (transfer of coracoid process to the glenoid defect) or a bone graft to the Hill-Sach’s lesion needs to be performed. These procedures require an open operation.
Physiotherapy
The patient may leave the hospital on the same day or the next day in case of an arthroscopic repair, and after 2-3 days after open surgery. The arm is placed in a shoulder immobilizer type of sling which restricts movement of the arm upwards, outwards and outward rotation of the arm. Depending upon the type of surgery performed and the strength of the repair achieved, the arm will be immobilized in the sling for a period of 3- 6 weeks. At around 2-3 weeks after surgery, pendulum exercises (gravity assisted movements of the arm) are initiated. At around 6 weeks after surgery, full range-of-motion exercises as well as shoulder strengthening exercises are started.
Overall it will take around 2-3 months after surgery for any patient to return to pre-operation status as far routine day-to-day activities are concerned. It may take around 3-4 months for a recreational athlete to return to sports, and even longer for a professional athlete (depending upon the nature of sport and the level of competition involved).
Website Designed By: Quick n Host