



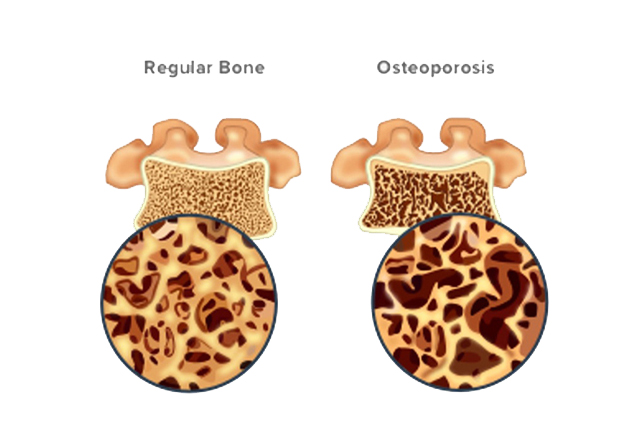
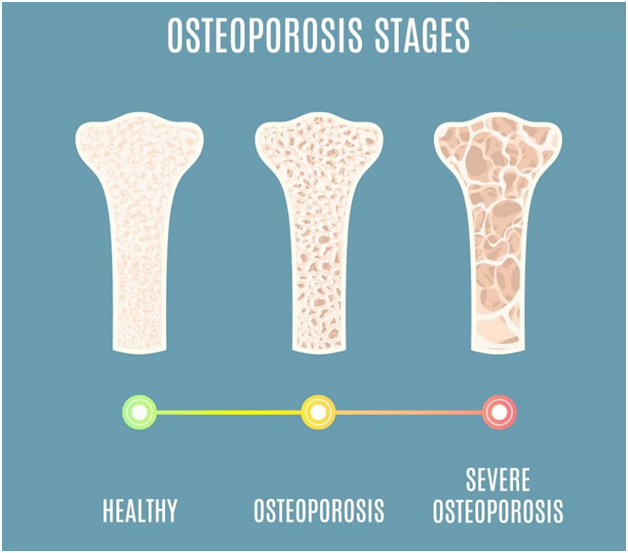
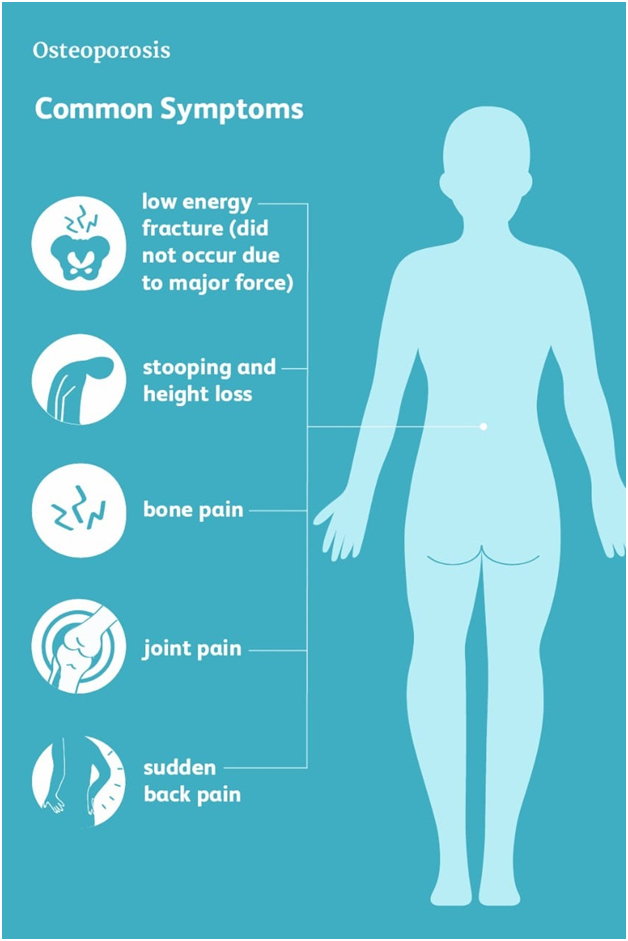
Osteoporosis, or porous bone, is a disease of progressive bone loss and skeletal deterioration in which bones become fragile and more likely to break, or fracture. The disease often develops unnoticed over many years, with no symptoms or discomfort, until a fracture occurs. Fractures at the hip, spine, and wrist are most common, although any bone can be affected. Many of these fractures are due a fall, however, even simple household tasks can produce a fracture of the spine if the bones have been weakened by the disease. These fractures often lead to chronic pain, disability and a reduced quality of life.
Fractures due to osteoporosis are common. One in two women and one in four men over age 50 will sustain a bone fracture in their remaining lifetime. Any bone can be affected, but of special concern are fractures of the hip and spine. A hip fracture almost always requires hospitalization and major surgery. Most hip fracture patients who previously lived independently will require help from their family or home care. Spinal or vertebral fractures also have serious consequences, including loss of height, severe back pain, and deformity.
The exact medical causes of osteoporosis are not completely known. However, many of the major factors that can lead to the disease have been identified, and are listed below:
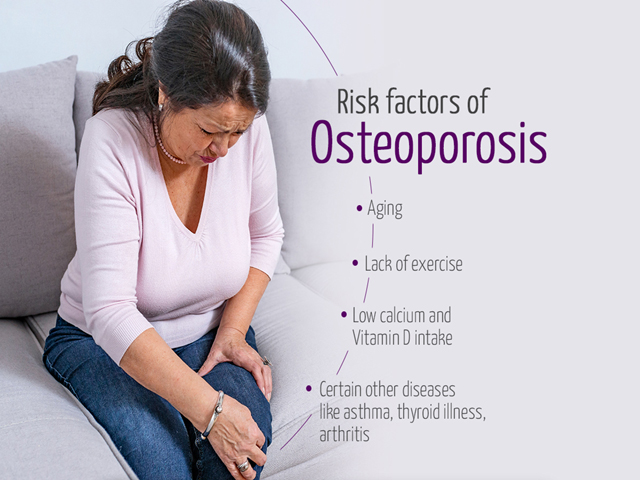
Everyone loses bone with age. After age 35, the body builds less new bone to replace losses of old bone. In general, the older you are, the lower your total bone mass and the greater your risk for osteoporosis
A family history of fractures; a small, slender body build; fair skin; and a Caucasian or Asian background can increase the risk for osteoporosis. Heredity also may help explain why some people develop osteoporosis early in life
Poor nutrition, including a low calcium diet, low body weight and a sedentary lifestyle have been linked to osteoporosis, as have smoking and excessive alcohol use.
Osteoporosis has been linked to some medications, including steroids, and to other illnesses, including some thyroid problems.
The diagnosis of osteoporosis is usually made by your doctor using a combination of a complete medical history and physical examination, skeletal X-rays, bone densitometry and specialized laboratory tests. If your doctor finds low bone mass, he or she may want to perform additional tests to rule out the possibility of other diseases that can cause bone loss, including osteomalacia (vitamin D deficiency) or hyperparathyroidism (overactivity of the parathyroid glands). Bone densitometry is a safe, painless X-ray technique that compares your bone density to the peak bone density that someone of your same sex and ethnicity should have reached at about age 20 to 25, when it is at it’s highest. It is often performed in women at the time of menopause.
There is a lot you can do throughout your life to prevent osteoporosis, slow its progression and protect yourself from fractures.
During the growing years, your body needs calcium to build strong bones and to create a supply of calcium reserves. Building bone mass when you are young is a good investment for your future. Inadequate calcium during growth can contribute to the development of osteoporosis later in life. However, whatever your age or health status, you need calcium to keep your bones healthy. Calcium continues to be an essential nutrient after growth because the body loses calcium every day. Although calcium can’t prevent gradual bone loss after menopause, it continues to play an essential role in maintaining skeletal health. Even if you’ve gone through menopause or already have osteoporosis, increasing your intake of calcium and vitamin D can decrease your risk of fracture. Dairy products, including yogurt and cheese, are excellent sources of calcium. An eight-ounce glass of milk contains about 300 mg of calcium. Other calcium-rich foods include sardines with bones and green leafy vegetables, including broccoli and collard greens. If your diet doesn’t contain enough calcium, dietary supplements can help. Talk to your doctor before taking a calcium supplement.
Vitamin D helps your body absorb calcium. According to a survey, 80 % of Indian population is deficient of vitamin D. The recommendation for vitamin D is 200-600 IU daily. Early morning sun exposure is the excellent source of vitamin D. Supplemented dairy products are also an excellent source of vitamin D. (A cup of milk contains 100 IU). But in the cases of severe deficiencies (proven by test), proper vitamin supplementation is required as guided by your doctor. Too much vitamin D can be toxic.
Like muscles, bones need exercise to stay strong. No matter what your age, exercise can help you minimize bone loss while providing many additional health benefits. We believe that a program of moderate, regular exercise (three to four times a week) is effective for the prevention and management of osteoporosis. Weight bearing exercises such as walking, jogging, hiking, climbing stairs, dancing, treadmill exercises, and weight lifting are probably best. Falls account for 50 percent of fractures, therefore, even if you have low bone density you can prevent fractures if you avoid falls.
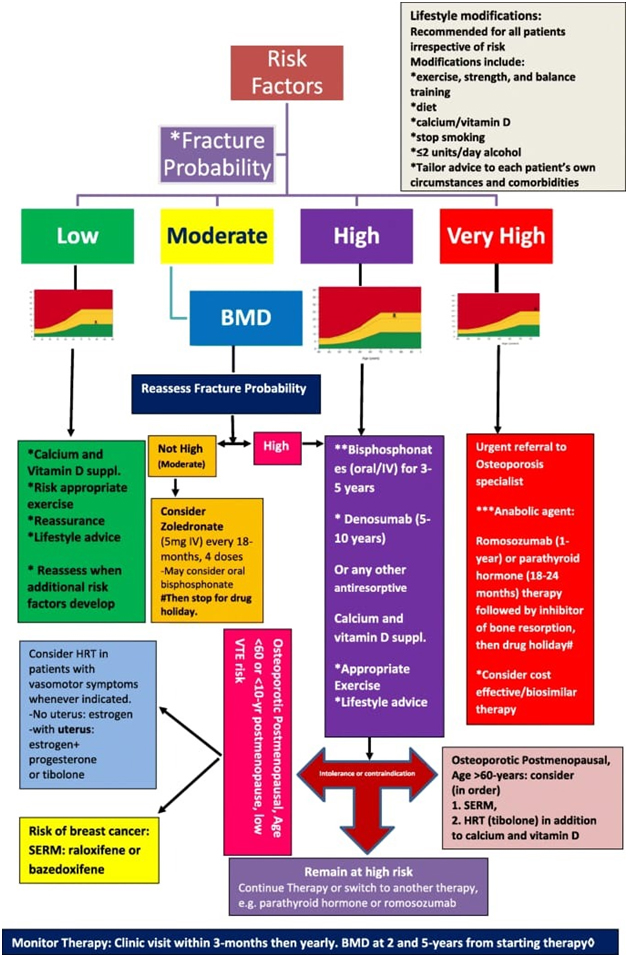
Although there is no cure for osteoporosis, there are steps you can take to prevent it, or to slow its progress. Treatment is often a team effort involving orthopaedist, gynecologist, physician and endocrinologist. a healthy diet, including adequate calcium and vitamin D, and healthy lifestyle, including adequate exercise, are important for maintenance of skeletal health. In some instances, medication may be useful for improving skeletal health. Currently several therapies are approved for the prevention and/or treatment of osteoporosis, including bisphosphonates (alendronate, risedronate, ibandronate, zolindronic acid), calcitonin nasal sprays, estrogens, selective estrogen receptor modulators (raloxifene), strontium ranelate, and parathyroid hormone (teriparatide inj). These agents have been shown to increase bone mineral density and reduce fracture risk in women with osteoporosis. Some of these therapies work mainly by slowing bone loss, whereas others promote new bone formation. If you and your doctor have decided that medical therapy is appropriate for prevention and/or treatment of your osteoporosis, it is critical that you follow the plan that you and your doctor have agreed to. Most people do not feel their bones getting stronger or weaker, so if you decide that a particular treatment is not right for you, please discuss your concerns with your doctor first, before stopping or interrupting your treatment.
Website Designed By: Quick n Host